Have you noticed swollen gums around your crown, or perhaps a dull ache near your dental restoration? A gum infection around a crown can cause not only irritation but also lead to more serious complications if left untreated. In fact, one study found that dental infection admissions in hospitals in the United States occur at a rate of 1 per 2,600 people.
Whether you’re dealing with inflamed gums around crown or mild gum pain around crown, understanding what’s happening is the first step in finding relief. In this guide, we’ll dive into the symptoms, causes, and treatment options for gum inflammation after crown placement, so you can take control of your oral health and avoid potential complications.
| Key Takeaways Gum infections around crowns occur when bacteria enter the soft tissue, often caused by poor hygiene or improper crown fitting. Common symptoms include swollen, tender gums, pain, redness, abscesses, and bleeding or pus. Infections are often caused by factors like poor hygiene, improper crown fitting, gum disease, or trauma to the area. At-home remedies like saltwater rinses and pain relief can help, but professional care like antibiotics or crown adjustments may be necessary. Seek professional help if symptoms worsen, persist, or if abscesses or pus appear to avoid serious complications. Prevent infections by maintaining good oral hygiene, visiting the dentist regularly, avoiding hard/sticky foods, and using a mouthguard if needed. |
What is a Gum Infection Around a Crown?
A gum infection around a crown occurs when bacteria enter the soft tissue around a dental crown, leading to inflammation, pain, and discomfort. Crowns, often made of porcelain, metal, or ceramic, are placed over damaged teeth to restore their shape, size, and function. However, while crowns are designed to last, they can sometimes create a small gap between the crown and the natural tooth, allowing bacteria to accumulate.
If oral hygiene isn’t maintained properly or if a crown isn’t fitted correctly, bacteria can seep beneath the crown and cause an infection. This leads to gum irritation around the crowned tooth, and in some cases, more serious conditions like abscesses. The infection can affect both the gums and the tooth underneath the crown, which may require professional treatment to prevent further damage.
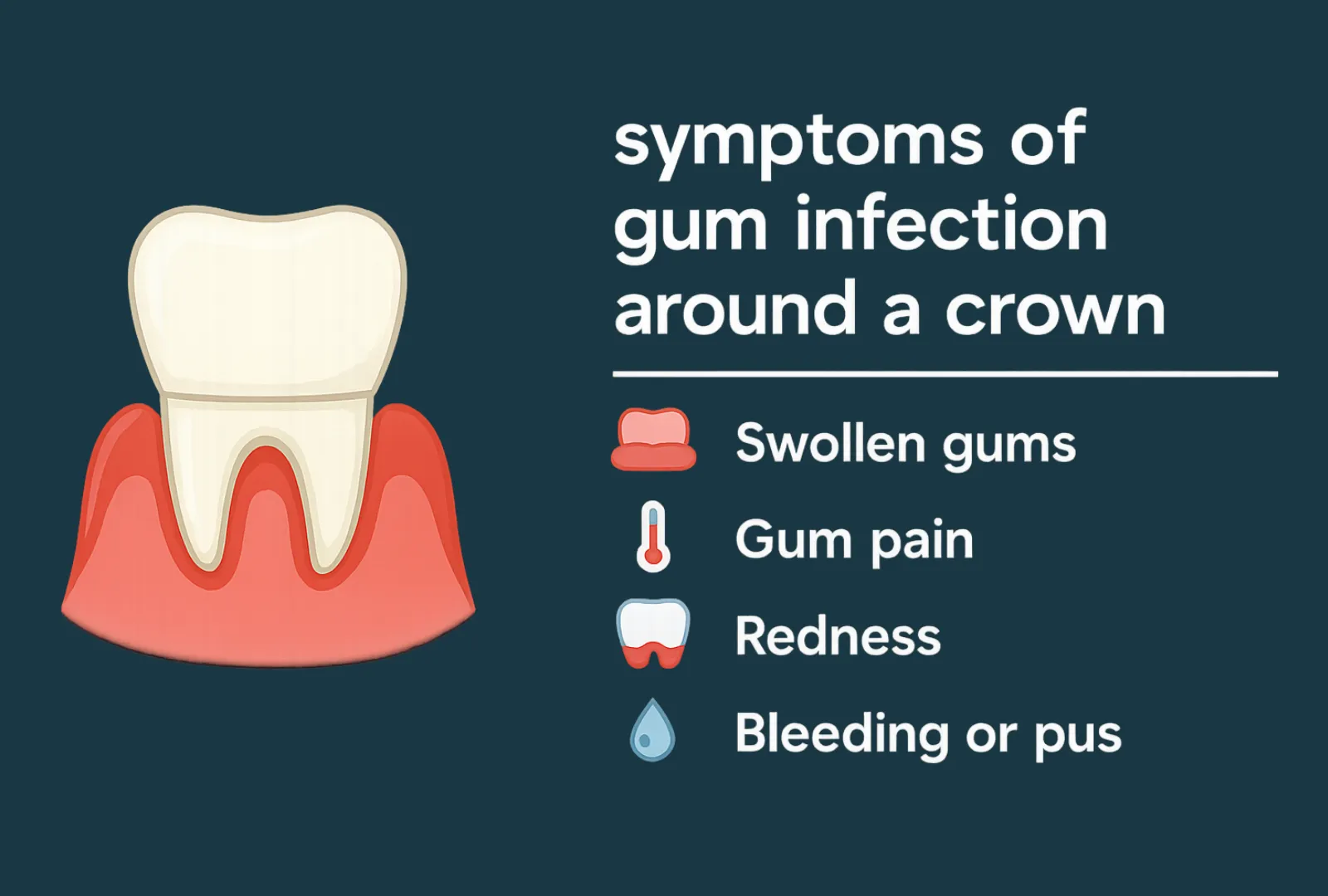
Symptoms of Gum Infection Around a Crown
When a gum infection around a crown develops, it’s usually accompanied by several noticeable symptoms. These symptoms can vary in severity, but the most common signs include:
- Swelling: The gums around the crown may become swollen and tender to the touch, which could indicate an infection.
- Pain: Mild to severe gum pain around the crown is common, especially when chewing or applying pressure to the affected area.
- Redness and Inflammation: The gums may appear redder than usual, and you may notice an increase in gum irritation around the crowned tooth.
- Abscess Formation: In some cases, an abscess may form, which is a pocket of pus that can develop around the infected gum tissue.
- Bleeding or Pus: If the infection worsens, you may notice bleeding when brushing or flossing, or even pus coming from the gums.
If these symptoms are left untreated, the infection can spread, leading to more severe complications such as gum inflammation after crown placement or even the potential loss of the crown.
Causes of Gum Infection Around a Crown
Several factors can contribute to a gum infection around a crown, and understanding these causes can help you prevent or address issues early. The most common causes include:
- Poor Oral Hygiene: One of the leading causes of infection around a crown is inadequate brushing and flossing. If food particles and plaque build-up along the gum line or under the crown, it can lead to bacterial growth and gum inflammation around crown.
- Improper Fitting of the Crown: If the crown doesn’t fit properly, it can create gaps between the crown and the tooth, where bacteria can thrive. This can lead to gum irritation after crown placement and ultimately to an infection if left unchecked.
- Gum Disease: Pre-existing conditions like gingivitis or periodontitis can make the gums more susceptible to infection. If you have gum disease, it can worsen around the crown and lead to painful symptoms like swollen gums.
- Trauma or Injury: Accidental damage to the crown or the surrounding area can lead to infection. Even slight trauma, such as chewing hard foods, may result in gum irritation around crown and expose the gums to bacteria.
- Weakened Immune System: People with compromised immune systems (due to illness or medication) may be at higher risk for infections, including those around crowns.
How to Treat a Gum Infection Around a Crown
If you’re experiencing symptoms of a gum infection around a crown, it’s important to take action promptly to avoid further complications. Here are some treatment options that can help:
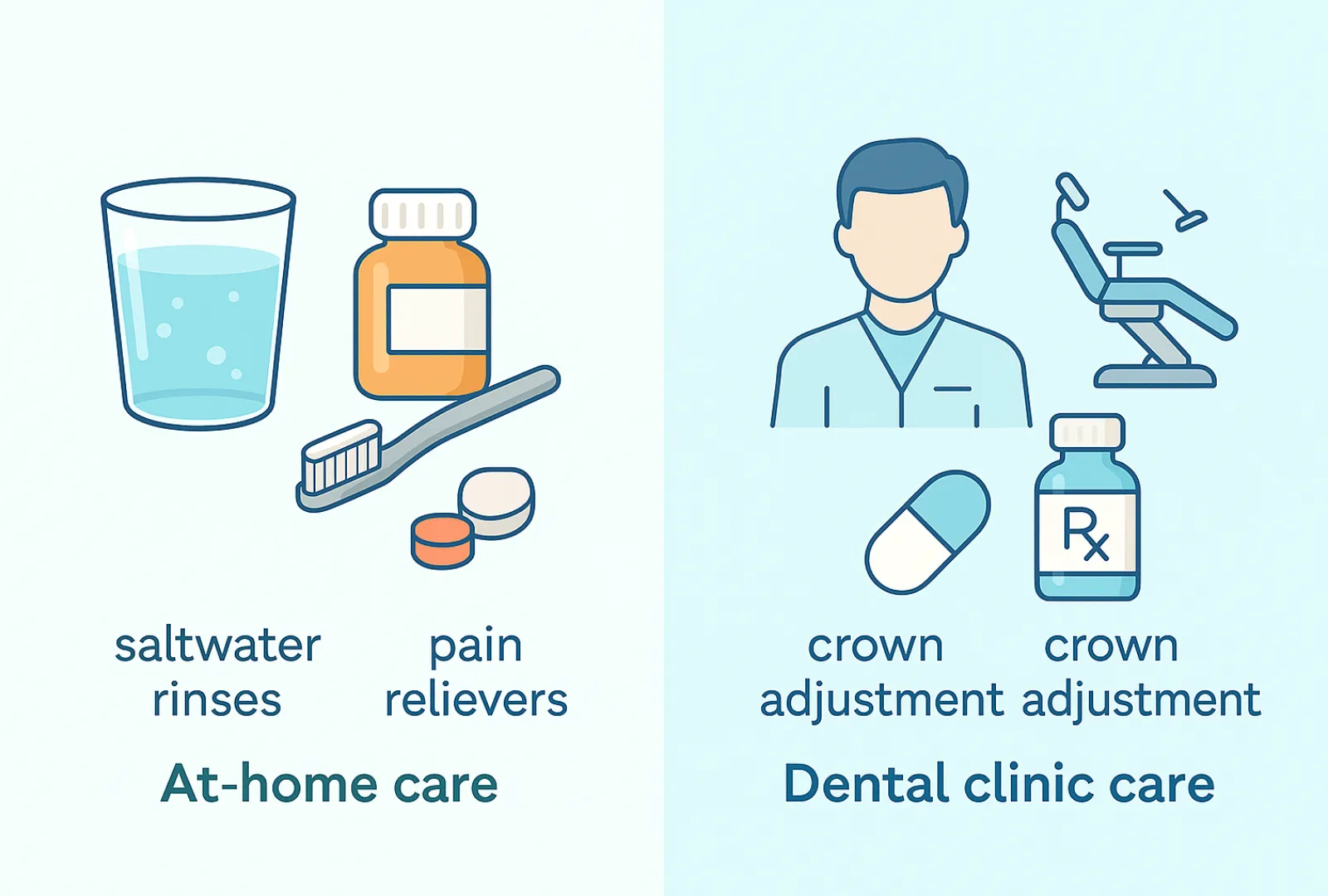
At-Home Remedies
For mild cases of gum inflammation around crown, several at-home remedies may help alleviate discomfort:
- Saltwater Rinses: Rinsing with warm saltwater is a simple and effective way to reduce swelling and discomfort caused by gum inflammation after crown placement. It helps to cleanse the area and may relieve mild symptoms. To prepare a saltwater rinse, mix half a teaspoon of salt into a cup of warm water and swish it around your mouth for about 30–60 seconds before spitting it out.
- Over-the-Counter Pain Relief: If you’re dealing with gum pain around the crown, medications like ibuprofen or acetaminophen can help reduce pain and inflammation. However, these should only be used temporarily until you can consult with a dentist.
| Can saltwater really help? While saltwater rinses can help soothe mild inflammation and reduce swelling temporarily, they cannot cure a gum infection. Saltwater is useful as a cleansing agent and to relieve discomfort, but persistent or severe infections require professional treatment, such as antibiotics or dental procedures. |
Dental Treatments
If your symptoms are more severe, or if at-home remedies don’t provide relief, it’s essential to seek professional dental care. A dentist can provide the following treatments to resolve the infection:
- Antibiotics: If the infection is bacterial, a dentist may prescribe antibiotics to clear it up. These may be taken orally or applied directly to the infected area.
- Crown Adjustment or Replacement: If the crown is improperly fitted or damaged, your dentist may need to adjust it or replace it to eliminate any gaps where bacteria can thrive. This can help prevent further gum irritation.
- Scaling and Root Planing: In cases where gum disease has contributed to the infection, a dentist may perform a deep cleaning to remove plaque and tartar buildup from under the crown. This procedure, known as scaling and root planing, helps restore gum health and reduce inflammation.
When to see a dentist
If any of the following occur, it’s important to see your dentist as soon as possible:
- If symptoms worsen or persist
- If there’s visible pus or abscess
- If the pain becomes severe
According to Christian Mehl, an internationally renowned implant surgeon and prosthodontics specialist, “If swelling or pain persists beyond a few days, it’s essential to seek professional dental treatment. Ignoring these symptoms can lead to more severe complications, including the risk of the infection spreading to the underlying bone.”
Don’t let a gum infection around a crown disrupt your smile. If you’re experiencing any of the symptoms above, it’s time to get professional help. Book your appointment with us today to get the care you need for a healthy, pain-free smile.
Preventing Gum Infection Around a Crown
Once you’ve treated any existing infections, it’s important to take steps to prevent future issues with your crowns. Here are some effective tips for maintaining healthy gums around your crowns:
- Maintain Proper Oral Hygiene: The most important factor in preventing a gum infection around a crown is consistent and thorough oral care. Brush your teeth at least twice a day with fluoride toothpaste and floss daily, especially around the edges of the crown, where bacteria can hide.
- Regular Dental Check-ups: Make sure to schedule regular visits with your dentist for check-ups and cleanings. These visits allow your dentist to monitor the condition of your crowns and detect early signs of infection or other issues.
- Avoid Hard or Sticky Foods: Hard foods can crack or damage crowns, and sticky foods can get trapped around the crown, leading to bacteria buildup. Being mindful of what you eat can reduce the risk of future infections.
- Use a Mouthguard: If you grind your teeth at night, consider using a mouthguard to protect both your crowns and your gums from unnecessary pressure and irritation.
Frequently Asked Questions
What are the best ways to treat a gum infection around a crown?
The most effective treatment for a gum infection around a crown involves both at-home remedies and professional dental care. At-home treatments like saltwater rinses and over-the-counter pain relief can help alleviate mild symptoms. However, if the infection persists or worsens, it’s important to visit your dentist for possible antibiotic treatment, a crown adjustment, or scaling to remove plaque buildup.
What does an infected crown look like?
An infected crown may cause symptoms like swollen gums around the crown, gum pain, redness, or the presence of pus. If the area around the crown becomes tender or if you notice an abscess forming, these could be signs of an infection. In some cases, the tooth underneath the crown may also be sensitive to pressure or temperature.
Is it possible for a gum infection to heal on its own?
In some cases, mild gum infections may resolve with proper oral hygiene and at-home treatments like saltwater rinses and pain relievers. However, more severe infections, especially those that involve pus or persistent pain, usually require professional intervention to ensure proper healing and prevent complications.
Can an infection under a crown resolve without professional treatment?
While some infections may improve with home care, an infection under a crown often requires professional treatment to prevent it from spreading or causing more serious issues. Your dentist may need to prescribe antibiotics or adjust the crown to eliminate gaps that allow bacteria to thrive.
