Did you know that nearly half of all adults in the U.S. suffer from some form of gum disease? According to the CDC, about 47% of adults, or roughly 64 million people, are affected by gum disease (periodontal disease). What’s more alarming is that the condition becomes more prevalent with age—approximately 70% of adults 65 and older have some form of gum disease. But can gum disease kill you?
While many brush off gum disease as a minor inconvenience, its impact can go far beyond what you might think. If left untreated, gum disease can lead to severe health complications, potentially even threatening your life. In this article, you will learn about the risks of gum disease, how it develops, why it can be serious, and most importantly, how to prevent it from becoming a life-threatening issue.
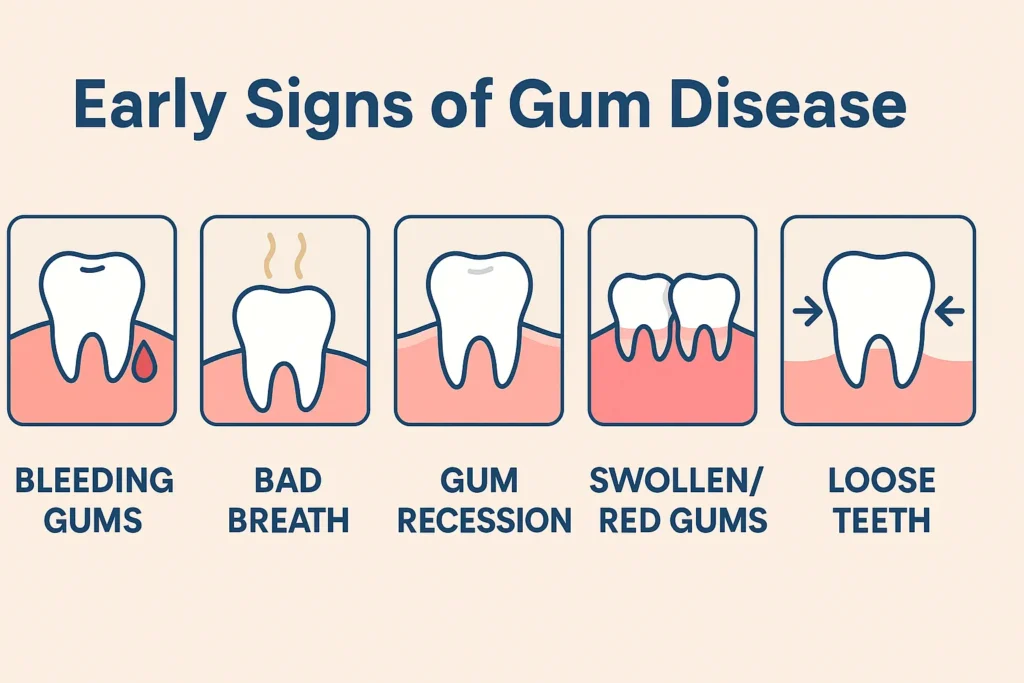
| Key Takeaways Gum disease can develop into periodontitis, a severe infection that affects the tissues supporting the teeth. If left untreated, it can lead to serious complications, including bone loss and receding gums. Bacteria from gum disease can enter the bloodstream, leading to systemic infections and contributing to conditions such as heart disease, stroke, and diabetes. Gum disease has been linked to an increased risk of cardiovascular disease, respiratory infections, and stroke. People with gum disease are nearly twice as likely to suffer from heart disease or stroke. Early signs of gum disease include bleeding gums, bad breath, gum recession, swollen or red gums, and loose teeth. Detecting these symptoms early can help prevent further damage and complications. Gum disease is preventable with regular brushing, flossing, eating a balanced diet, and quitting smoking. Seeing a dentist promptly for treatment and following their care plan is crucial for maintaining gum health and preventing serious conditions. |
What Is Gum Disease and How Does It Develop?
Gum disease, also known as gingivitis in its early stages, can develop into a more severe condition called periodontitis if left untreated. It is an infection of the tissues that support your teeth, caused by the buildup of plaque and bacteria. Here’s how it typically develops:
- Gingivitis: In the early stages, plaque builds up along the gumline, causing irritation and inflammation in the gums. At this point, you may notice symptoms like redness, swelling, and bleeding, especially when brushing or flossing.
- Periodontitis: If gingivitis goes untreated, it progresses into periodontitis, where the inflammation spreads deeper into the gum tissue and may begin to affect the bone structure that holds the teeth in place.
Key factors that contribute to gum disease:
- Poor oral hygiene: Inadequate brushing and flossing allow plaque and tartar buildup, which can lead to gum disease.
- Smoking: Smoking weakens your immune system, making it harder for your body to fight off infections, including gum disease.
- Genetics: Some people are more predisposed to gum disease due to their genetic makeup.
- Medical conditions: Conditions like diabetes or certain medications can increase the risk of developing gum disease.
Can Gum Disease Kill You? The Serious Risks
So, can you die from gum disease? The short answer is yes. However, while gum disease itself may not directly cause death, leaving it untreated can result in life-threatening complications. Bacteria from infected gums can enter the bloodstream and contribute to serious conditions such as heart disease, stroke, and diabetes. As the disease advances, it may also result in receding gums, the formation of gum pockets, and bone loss. These systemic infections can worsen existing illnesses or even trigger new ones, including:
- Cardiovascular disease
- Respiratory infections
- Stroke
The Link Between Periodontitis and Other Serious Health Conditions
Here’s how gum disease affects other parts of the body and contributes to major health risks:
Cardiovascular disease
Periodontal disease has been strongly linked to an increased risk of heart disease. The bacteria from infected gums can enter the bloodstream, leading to inflammation in the arteries, which may contribute to the buildup of plaque. This, in turn, increases the risk of heart attacks and strokes. According to the American Heart Association, individuals with gum disease are nearly twice as likely to suffer from heart disease as those with healthy gums. In fact, studies have shown that people with severe gum disease are more likely to experience clogged arteries, which can lead to heart complications.
Diabetes
Poor oral health can make it harder to control blood sugar levels, while high blood sugar can make you more vulnerable to infections like periodontitis. According to the Centers for Disease Control and Prevention (CDC), people with diabetes are more likely to develop gum disease, and those with gum disease may find it harder to manage their diabetes. In fact, studies show that more than 90% of people with diabetes have some form of oral health issue, and gum disease is a common problem among them. This is because diabetes can severely damage the tissues in the mouth, leading to more serious periodontitis. If left untreated, gum disease can make it even harder for diabetics to keep their blood sugar under control, creating a dangerous cycle.
Respiratory diseases
The bacteria from gum disease can travel to the lungs, leading to infections like pneumonia or chronic obstructive pulmonary disease (COPD). Studies show that people with periodontitis are more likely to develop these respiratory conditions. One study found that gum disease was more common in people with COPD (26.5%) compared to those without it (22.2%). In fact, those with COPD are about 21% more likely to have gum disease. Since COPD affects around 16 million Americans, this shows how gum disease can contribute to serious lung problems.
Stroke
A stroke occurs when blood flow to the brain is interrupted, and studies have shown a connection between periodontitis and an increased risk of stroke. The bacteria from gum disease can lead to inflammation and the buildup of plaque in the arteries, which could eventually cause a stroke. The American Heart Association indicates that individuals with gum disease are twice as likely to suffer from a stroke as those with healthy gums. In fact, stroke is the fifth leading cause of death in the United States, and many stroke survivors have underlying gum disease.
Early Signs of Gum Disease and What You Should Watch For
It’s important to spot gum disease early so you can prevent it from getting worse. Here are some early signs to look out for:
- Bleeding gums: If your gums bleed when you brush or floss, it’s a sign that your gums are inflamed and irritated.
- Bad breath: Persistent bad breath, also known as halitosis, can be a sign of gum infection or poor oral hygiene.
- Gum recession: If your gums start to pull away from your teeth, exposing more of your tooth or even the root, it’s a sign of gum disease.
- Swollen or red gums: Healthy gums should be pink and firm. If they’re swollen, red, or tender to the touch, that could be a sign of gum disease.
- Loose teeth: Advanced gum disease can loosen teeth or even cause them to fall out.
| Is gum disease only a problem for older adults? Although gum disease is more common among adults aged 65 and older, it can affect anyone, regardless of age. Poor oral hygiene, smoking, genetics, and certain medical conditions make people of all ages vulnerable to gum disease. Early detection and proper oral care are essential at any age to prevent serious complications later on. |
How is Periodontal Disease Treated
When diagnosed early, periodontal disease can be managed effectively with a combination of non-surgical and, in advanced cases, surgical treatments. Let’s take a closer look at the treatment options for periodontal disease:
Non-Surgical Treatments
Non-surgical treatments are often the first line of defense in treating periodontal disease. These methods aim to remove plaque and bacteria from below the gumline, helping to restore gum health and prevent further damage. One of the most common non-surgical treatments is scaling and root planing, which involves cleaning the teeth and smoothing the root surfaces to remove tartar and bacteria.
Antimicrobial treatments: In some cases, antimicrobial agents, such as mouth rinses or gels, may be prescribed to reduce bacterial infection and inflammation in the gums.
Surgical Options for Advanced Periodontal Disease
If non-surgical treatments are not sufficient, surgical intervention may be required for more severe cases of periodontitis.
- Flap surgery: This procedure involves lifting back the gums to remove tartar buildup and then suturing the gums back into place. It helps in restoring a healthier gum tissue around the teeth.
- Bone grafting: In some cases where the bone has been damaged by gum disease, bone grafting may be used to regenerate bone tissue and restore tooth support.
The Role of Antibiotics
Antibiotics can be essential in controlling infection, especially when gum disease has led to significant bacterial growth. They may be administered in various forms—oral antibiotics or topical applications—to reduce infection and promote healing in the affected areas.
Preventing Gum Disease and Protecting Your Health
The good news is that gum disease is preventable with the right care. Here are some simple steps to keep your gums healthy and avoid serious complications:
- Brush and floss regularly: Brush your teeth at least twice a day and floss daily to remove plaque and bacteria from between your teeth and along the gumline.
- Eat a balanced diet: Foods rich in vitamins and minerals, like fruits, vegetables, and dairy, help maintain strong, healthy gums.
- Quit smoking: Smoking is a major risk factor for gum disease, so quitting can significantly reduce your risk.

What to Do If You Suspect Gum Disease?
If you notice any signs of gum disease, don’t wait for it to get worse. Here’s what you should do:
- See a dentist right away: If you notice bleeding gums, bad breath, or any other signs of gum disease, make an appointment with your dentist. They will examine your gums and determine the best treatment.
- Follow your dentist’s treatment plan: Your dentist may recommend professional cleaning (scaling and root planing) to remove plaque and tartar buildup. In some cases, antibiotics or other treatments may be prescribed to fight the infection.
Are you noticing signs of gum disease? Don’t wait—schedule your dental checkup today and take the first step toward healthier gums and overall health. Book your appointment now!
Frequently Asked Questions
How long can you live with gum disease?
With proper treatment and care, gum disease can be managed for many years. However, if left untreated, it can worsen and lead to severe complications. Early intervention is key to preventing further damage.
What are the initial signs of a gum infection?
The first stage of a gum infection, gingivitis, includes symptoms like swollen, red gums, bleeding when brushing, and bad breath. These can often be reversed with good oral hygiene.
Can gum disease be completely cured?
While early-stage gum disease can be reversed, advanced periodontitis cannot be fully cured. Treatment can manage the condition and prevent further damage.
How does a dentist diagnose gum disease?
Dentists diagnose gum disease through a thorough exam, measuring gum pocket depth and checking for signs of inflammation and bone loss. X-rays may be used to assess damage.
